OSU scientists helping to seek cure for tuberculosis
Wednesday, October 5, 2022
Oklahoma State University and the Oklahoma Center for Respiratory and Infectious Diseases (OCRID) are teaming up through a National Institutes of Health grant to take the first steps in curing Mycobacterium tuberculosis.
Tuberculosis is one of the deadliest infections in the world with 10 million active infections each year and 1.4 million deaths in 2019, according to the World Health Organization.
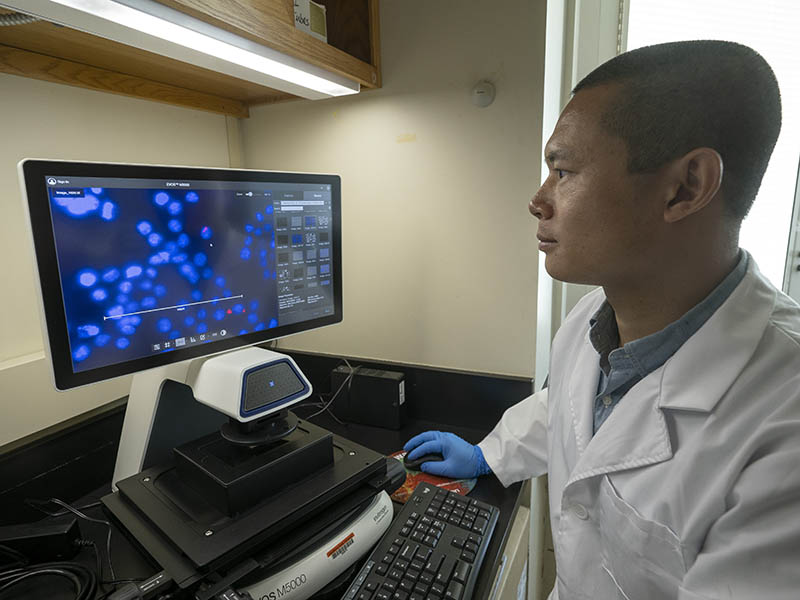
“It is important to understand the mechanism that causes TB in humans. We are studying how immune cells fight against tuberculosis,” said Yong Cheng, an assistant professor in the OSU Department of Biochemistry and Molecular Biology. “Additionally, to better control global TB spread, it is necessary to understand immune defense. The focus of our study is to understand the immune response in humans as a means to cure TB.”
Both the immune system and the bacteria that cause TB determine the outcome of the infection, according to Cheng. The long-term goal of the study in his laboratory is to identify host lncRNAs that are beneficial to immune defense against TB infection and to further understand how lncRNAs help regulate host immunity.
Data from previous research showed that a group of host molecules called long noncoding RNAs (lncRNAs) plays an important role in the immune defense of microbial infections, but there is limited knowledge on their role when it comes to TB specifically.
OCRID recently developed a gene-editing screening technique to study lncRNAs in human cells.
“In collaboration with them, we are using this new technique to identify host molecules that can activate the immune response to kill Mycobacterium tuberculosis,” Cheng said. “Our aim is to screen and develop new therapeutic tools and techniques that can be used to treat TB disease in humans.”
Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under award number 1R21AI166118-01A1 through the exploratory/developmental research grant (R21). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The project is also supported by the OCRID CoBRE grant and the OCRID center mentorship program, which provides training and mentoring to junior faculty and the next generation of scientists.